The Breast Is Yet To Come – Breast Changes and Red Flags
Breasts are just like any other part of our body – prone to changes throughout our lifetime. However, it’s also important to know that breast are unique structures that follow a distinct pattern of anatomical development – let’s dive into the science, from A to Z!
Development of Breasts in The Womb
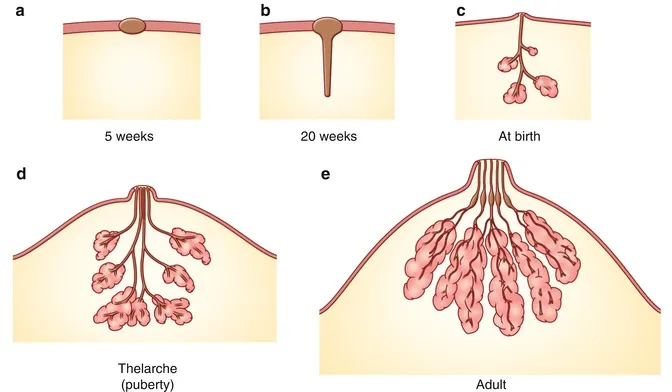
Breast development begins during the 4th week of development in the womb!
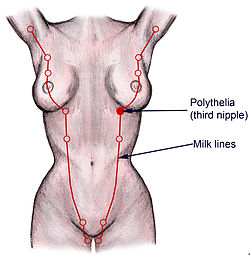
Two symmetrical “Mammary Ridges” (a.k.a. milk lines) form along each side of the embryo, stretching from the armpit to the groin.
Mammary Ridges (4-6 weeks): These ridges give rise to the future breasts. In humans, only a small section of the ridge, located in the chest area, persists, while the rest disappears. (If the rest do not disappear, they form what are known as “Supernumerary Nipples“, which look like moles along the milk line! If the growth persists and forms tissue, it is called as “Polymastia“.)
Primary Bud Formation (6-8 weeks): The mammary ridge thickens in the chest region, forming a Primary Mammary Bud that will eventually become the breast tissue.
Secondary Bud Formation (8-12 weeks): The primary bud branches into secondary buds, which penetrate into the surrounding mesenchyme. These secondary buds will develop into the milk ducts.
Canalization (3rd trimester): The secondary buds hollow out to form lactiferous ducts, which open into a central mammary pit (the future nipple area).
At birth, the breast consists of simple lactiferous ducts.

Development of Breasts During Puberty
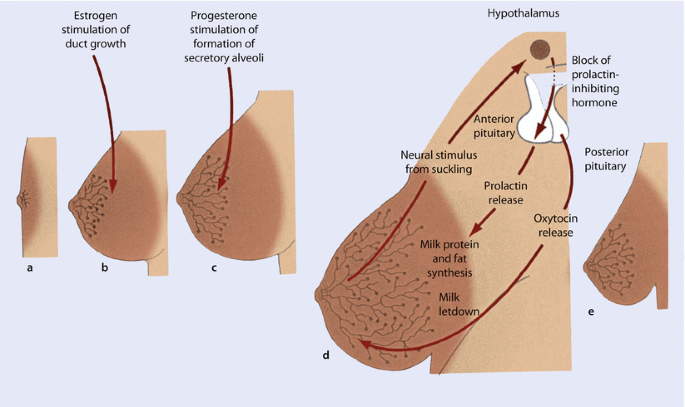
Further development: like glandular tissue growth, occurs during puberty under the influence of hormones like estrogen and progesterone. This is when the typical anatomy of male versus female breasts begins to differ. In certain cases, male breasts might also be affected by the hormones, giving rise to a condition called “Gynecomastia“.
Puberty: Estrogen promotes ductal growth, while progesterone aids in the formation of the lobules and alveoli, essential for future milk production.
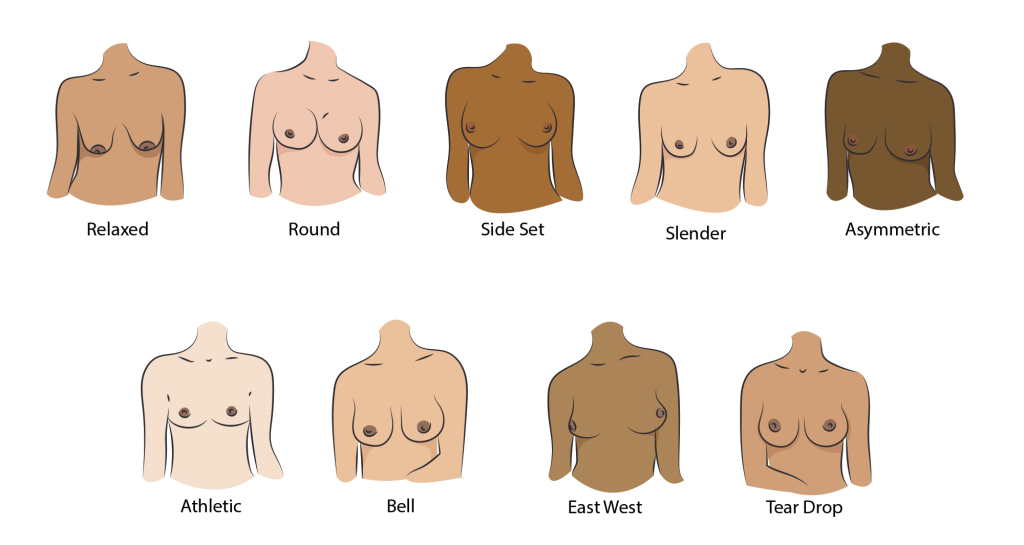
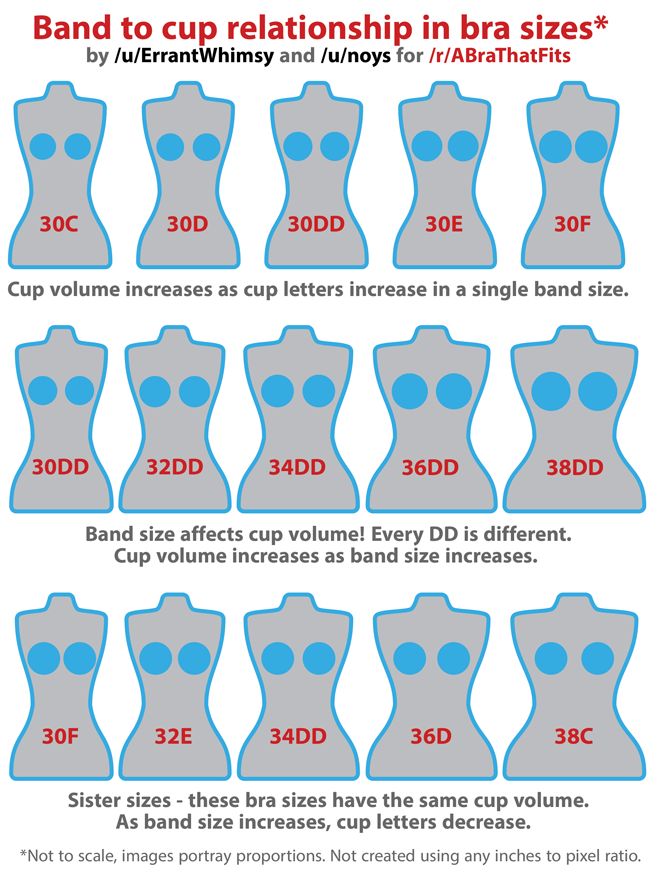
- Semi-permanent characteristics of breasts form during this phase, like size, shape, and color.
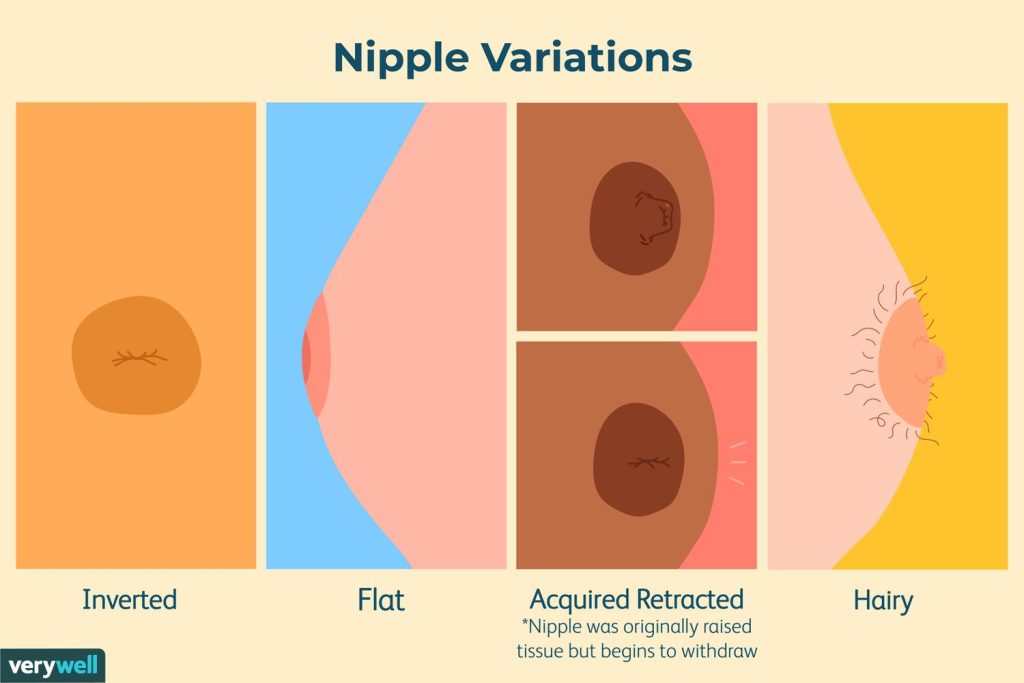
- While most breasts look similar, there can be variations in features like nipples, and others!
- It is important to note that there is no perfect breast, and all breasts are equally beautiful! Take a deeper look here.
Development of Breasts During Pregnancy and Breast Feeding
1. Hormonal Influence
The main hormones involved in breast changes during pregnancy and lactation include:
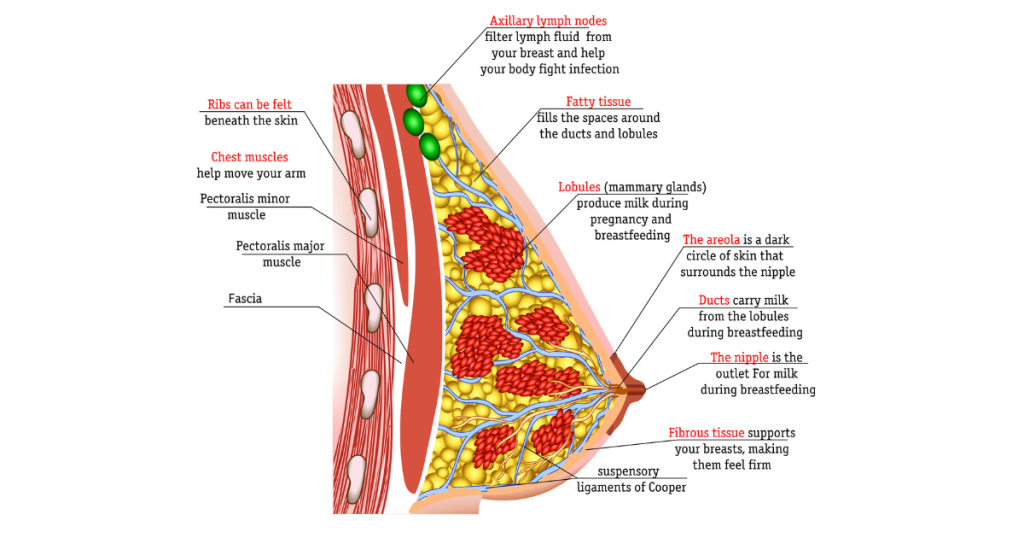
Estrogen: Promotes the growth of the milk ducts.
Progesterone: Aids in the development of the milk-producing glands (lobules and alveoli).
Prolactin: Stimulates milk production after birth.
Oxytocin: Facilitates the let-down reflex, helping milk flow from the alveoli to the nipple.
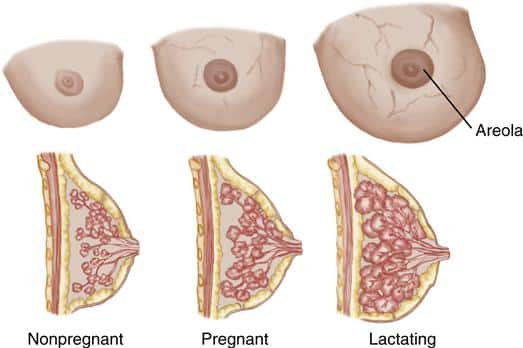
2. Changes During Pregnancy
First Trimester
Growth of Milk Ducts: Estrogen levels rise, stimulating the ducts to grow and branch out.
Increased Blood Flow: Breasts may feel tender, warm, and swollen due to increased blood flow.
Darkening of Areolae: The areola becomes larger and darker, a change that is thought to help the newborn find the nipple for breastfeeding.
Second Trimester
Lobule and Alveoli Growth: Progesterone stimulates the formation of milk-producing lobules and alveoli. Breasts may continue to increase in size.
Colostrum Production Begins: Colostrum, a thick, nutrient-rich fluid that will be the baby’s first food, may begin to be produced in small amounts.
Increased Fatty and Glandular Tissue: Breasts become fuller as glandular tissue replaces some fatty tissue, preparing for milk production.
Third Trimester
Final Gland Development: The milk-producing glands reach their full development. The alveoli are now capable of producing milk.
Leaking Colostrum: Some people may notice small amounts of colostrum leaking from the nipples as birth approaches.
Breast Sensitivity: Breasts can become more sensitive or tender as the body prepares for lactation.
3. Postpartum Changes (Lactation)
Initiation of Milk Production
After Birth (Day 1-3): When the placenta is delivered, there is a sudden drop in progesterone and estrogen, which triggers prolactin to start milk production. Colostrum is secreted for the first few days postpartum. This fluid is good for enhancing the immunity of the baby and must not be thrown away.
“Milk Coming In” (Day 3-5): Mature milk production begins, causing the breasts to feel fuller, heavier, and sometimes engorged. This transition from colostrum to mature milk is sometimes referred to as the “milk coming in.”
Maintenance of Milk Supply: Milk production works on a supply-and-demand basis. The more the baby nurses, the more milk is produced. Emptying the breasts (either through breastfeeding or pumping) signals the body to produce more milk.
Oxytocin and Let-Down Reflex: When the baby suckles, oxytocin is released, triggering the let-down reflex, which allows milk to flow from the alveoli through the milk ducts to the nipple.
4. Structural Changes
Lobules and Alveoli Expansion: During lactation, the alveoli (small sacs where milk is produced) expand and fill with milk, while the surrounding lobules and ducts enlarge to accommodate the increased milk flow.
Nipple and Areola Adaptation: Nipples often become more pronounced, and the areola remains darkened, which aids the baby in latching.
5. Breast Involution (After Weaning)
Once breastfeeding stops (weaning), the breasts undergo a process called involution, where the glandular tissue shrinks and the breast gradually returns to its pre-pregnancy state. This process can take several weeks to months, and some changes may persist, such as less firmness or slight sagging due to the stretching of the skin and tissues.
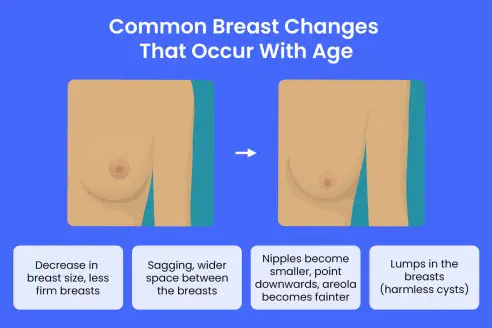
Development of Breasts in Old Age
1. Loss of Firmness and Sagging (Ptosis)
Reduced Elasticity: The connective tissues (Cooper’s ligaments) that support the breasts lose elasticity over time, causing sagging.
Decreased Glandular Tissue: With aging, glandular tissue (which produces milk) is gradually replaced by fatty tissue, leading to a softer, less firm appearance and feel.
Gravity: Over the years, the effect of gravity contributes to the stretching of skin and ligaments, further causing the breasts to droop.
2. Size and Shape Changes
Decrease in Breast Size: Post-menopausal hormonal shifts, especially the reduction in estrogen, can lead to a decrease in overall breast size as glandular tissue shrinks.
Asymmetry: Breast asymmetry may become more noticeable as the size and shape of each breast change independently over time.
Flattening: The once fuller and rounder breast shape may give way to a flatter, elongated appearance due to the loss of tissue volume and elasticity.
3. Changes in Skin
Thinning and Wrinkling: The skin covering the breasts becomes thinner, drier, and more prone to wrinkles with age due to decreased collagen production.
Loss of Fat: Breasts lose some of the subcutaneous fat, making them feel less plump or full.
4. Nipple and Areola Changes
Nipple Position: Nipples may point downward or flatten due to the sagging of the breast tissue.
Areola Size: The areola (the pigmented area around the nipple) may shrink in size and become less distinct.
Color Changes: The areola and nipple can become paler, with less pronounced pigmentation as hormone levels decline.
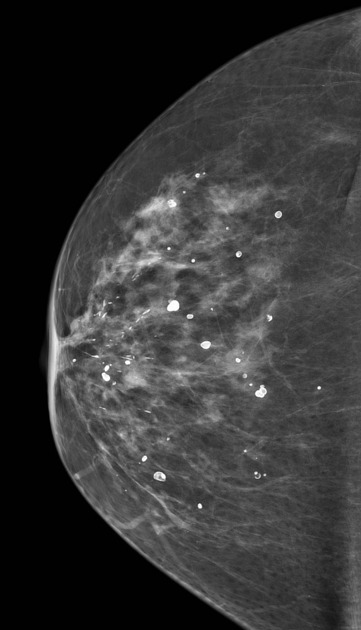
5. Changes in Breast Density
Decreased Density: Breasts become less dense as glandular tissue (which is denser) is replaced by fatty tissue. This is why older individuals tend to have softer, less firm breasts.
Impact on Mammograms: With decreased breast density, mammograms in older women may show clearer results, as fatty tissue is easier to examine than dense glandular tissue.
6. Hormonal Influence
Post-Menopausal Changes: After menopause, the drop in estrogen causes the most significant changes in breast tissue. The glandular component shrinks, and fat becomes the primary tissue, resulting in less fullness.
Reduction in Sensitivity: Some people experience reduced sensitivity in the breasts and nipples due to hormonal changes and aging.
7. Lumps and Other Abnormalities
Benign Lumps: Older individuals may develop benign breast conditions like cysts or fibroadenomas, but it’s still important to monitor any new lumps.
Increased Cancer Risk: The risk of developing breast cancer increases with age, making regular breast exams and mammograms essential.
8. Calcium Deposits (Microcalcifications): Small calcium deposits may develop in the breast tissue, often seen on mammograms. These are usually harmless but may sometimes warrant further investigation, as they can be associated with early stages of breast cancer.
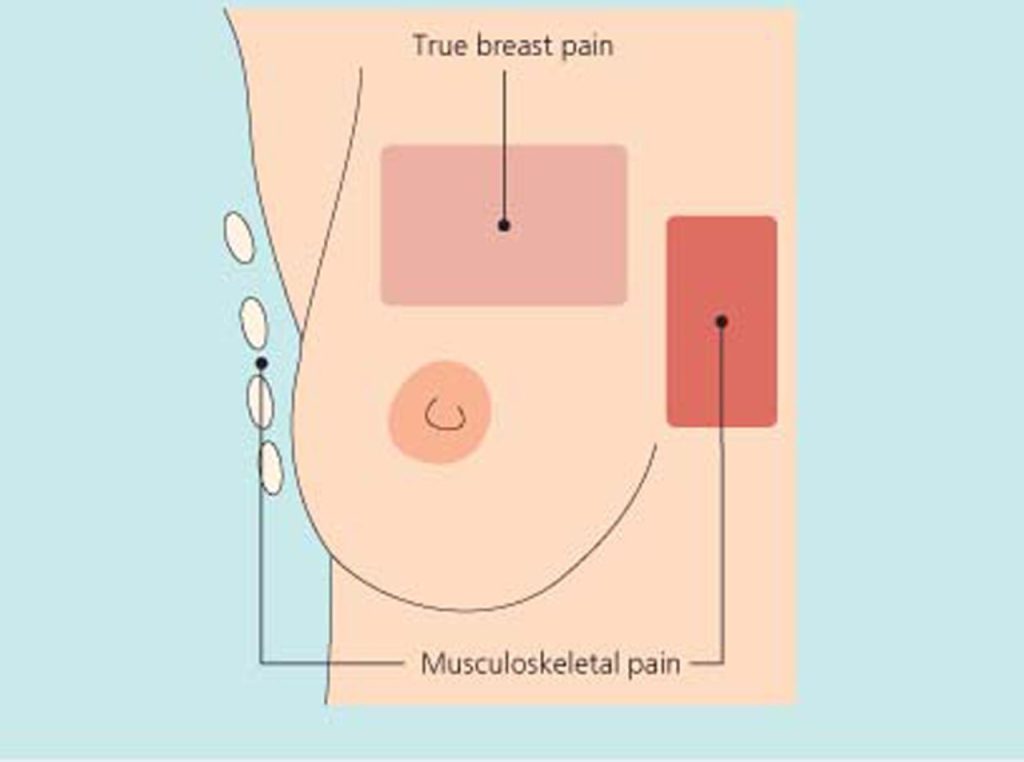
9. Breast Pain or Discomfort (Mastalgia): While less common post-menopause, some people may still experience occasional breast pain, usually linked to hormonal treatments or benign conditions like cysts.
10. Changes in Lymphatic Tissue: Lymphatic drainage may become less efficient with age, leading to a higher chance of fluid retention, swelling, or the development of benign lumps.
11. Increased Risk of Conditions
Breast Cancer: Age is one of the most significant risk factors for breast cancer, and older individuals should continue regular mammograms as recommended by their healthcare provider.
Benign Breast Diseases: Conditions like ductal ectasia (widening of the milk ducts) and benign lumps may be more common in older women due to changes in breast tissue composition.
12. Post-Surgical or Treatment Changes
Impact of Surgery or Radiation: If a person has had breast surgery (e.g., mastectomy, lumpectomy) or radiation therapy for breast cancer, the affected breasts may have additional changes like scar tissue, loss of symmetry, or alterations in sensation.
Red Flag Changes to Look Out For🚩
1. New Lumps or Masses
2. Changes in Breast Size or Shape
3. Skin Changes
4. Nipple Changes
5. Pain or Discomfort
6. Unexplained Changes in Texture
7. Unusual Vein Patterns
8. Swelling or Lumps in the Armpit
9. Persistent Itchiness
10. Unexplained Weight Loss or Fatigue
11. Non-Healing Sores
12. Rapid Increase in Breast Size (Non-Pregnancy)
If you notice any of these red flags or any other unusual changes in your breasts, it’s essential to consult a healthcare professional for a comprehensive evaluation.
Early detection of problems, including breast cancer, significantly improves outcomes. Regular breast self-exams and routine mammograms (as recommended based on age and risk factors) are critical in catching potential issues early.
Stay healthy and remember: all breasts are breautiful!
Author


1 thought on “The Breast Is Yet To Come – Breast Changes & Red Flags”
Well-written! Very informative..