Dissecting the Stigma: Cervical Cancer and its Types
Cancer is one of the leading causes of death worldwide, especially in India, a huge number of people die due to cancer each year. While these deaths are covered extensively by mainstream media and also find a place in our day to day conversations, deaths by cervical cancer are an extremely taboo topic in India. They are a major cause of death amongst females in their 30s and are often ignored because it is caused by sexual activities. As a result, many people do not even seek professional help, and even if they do, they are not open about their treatment process, fearing alienation by society.
What is Cervical Cancer?
Cervical Cancer refers to cancer of the cervix i.e the connecting duct between the uterus (where the fetus develops) and the vagina. (the opening through which menstruation/natural delivery occurs) The cervix has two parts –
- The Endo-cervix – Made up of glandular cells
- The Exo-cervix – Made up of squamous cells
The zone where the endocervix starts and the exocervix ends, or the meeting place of these two cells, is the transformation zone, where cervical cancer usually begins. It occurs due to the passage of HPV (Human Pappilomavirus) which is often transmitted from one person to the other during sexual activities. However, studies indicate that the passage of HPV alone rarely results in cervical cancer – unhealthy habit patterns put women at a greater risk of contracting the disease.
Cervical cancer can broadly be classified into three major types on the basis of their place of origin in the body-
- Squamous Cell Carcinomas – The most common form of cervical cancer, it originates in the cells of the exo-cervix.
- Adenocarcinomas – It develops in the mucus generation glandular cells of the cervix
- Mixed Carcinomas – It is less common compared to the other two types and has features of both squamous and adeno carcinomas
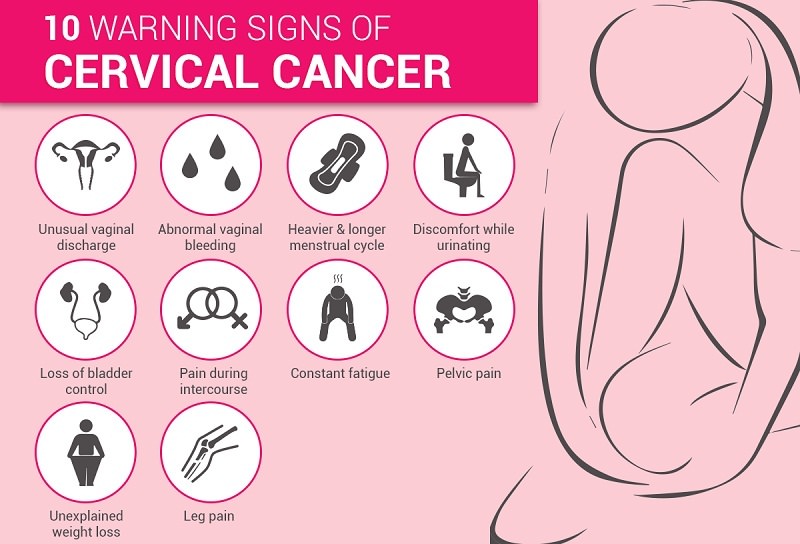
What are the Symptoms of Cervical Cancer?
Symptoms of cervical cancer are usually observed only in advanced cases, which is why it is harder to detect it at an earlier stage. In fact, the only way it can be detected is by regular screening check-ups. While these symptoms might not always point towards cervical cancer it is extremely important to get yourself checked, to prevent cancer from growing into an even more advanced stage. Some symptoms that are observed in the advanced stage include –
- Vaginal bleeding post sexual activities
- Unusual nature of vaginal discharge
- Constant pain during sexual activities
- Swelling in the legs or the pelvic region, marked by an unpleasant sensation
- Passage of blood along with the urine
Can Cervical Cancer be prevented?
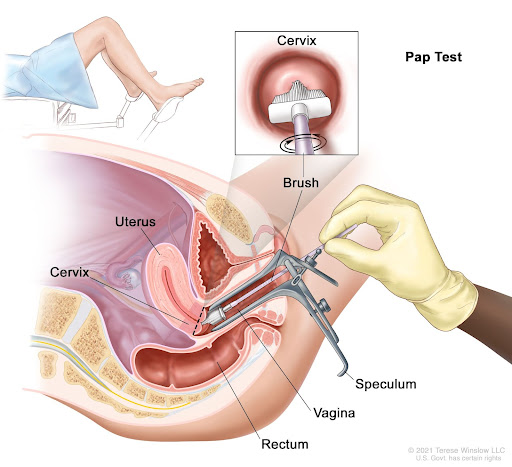
The transformation of cells in the cervix does not take place overnight, it takes anywhere between 3 to 5 years for them to develop into cancer and if detected at an earlier stage this conversion can be limited to a great extent. Ideally, one should start going for regular screening checks every 2-3 years after they become sexually active or at the age of 21, regardless of whether they are sexually active or not. The process includes cervical cytology (or a pap test) or an HPV test. Another naval method of preventing the contraction of cervical cancer includes HPV vaccines.
In the case of pap tests, a line of cells is smeared from the cervix, which is then kept under observation to detect any abnormalities. In case of an HPV test, the sample is tested for the virus. While having the screening test every 3 years is effective for most, people who have a history of HIV or have a weakened immune system may need to get themselves tested every year due to a higher risk. In certain cases, your screen test may indicate false positives or false negatives, and in order to prevent these occurrences as much as possible, you should avoid sexual intercourse and vaginal products two days before your appointment.

Conclusion
Analysis of global health reports all indicate that while screening is the most accurate tool for the prevention of the disease, the number of people that actually resort to screening is extremely low. This is due to the belief that most people have regarding the disease itself – it is often linked with incautious sexual activities by the common people, and people with cervical cancer are often sl*tshamed. Thus, stereotypical gender and societal norms need to be challenged and conversations around HPVs ought to be initiated for a more inclusive and informed environment.
Cover Illustration: flo.health
Author