Early Detection Saves Lives
Arshia Bathla writes, the National Breast Cancer Foundation reminds us that 2020 has been a year that has made us realize, now more than ever, that we’re all in this together, and our choices and actions help us protect each other. This rings true in the theme that ‘Early detection saves lives.’
The National Breast Cancer Foundation reminds us that 2020 has been a year that has made us realize, now more than ever, that we’re all in this together, and our choices and actions help us protect each other. This rings true in the theme that ‘Early detection saves lives.’
According to WHO, there are about 1.38 million new cases and 458,000 deaths from breast cancer each year (IARC Globocan, 2008). Breast cancer is by far the most common cancer in women worldwide. It is reported that every four minutes, an Indian woman is diagnosed with breast cancer. A 2018 report of Breast Cancer statistics recorded 1,62,468 new registered cases and 87,090 reported deaths.
The survival rates of breast cancer in India are low because the detection takes place late, one way to change these numbers is by increasing awareness. Breast cancer is a treatable disease and chances of survival are higher if it’s detected in time, thus making it important to be aware of the means to detect it.
Early Detection?
In a study conducted in Kerala in 2019, it was found that early detection is an important strategy in low and middle-income countries for improved survival and simple cost-effective treatment. In India, a breast lump is often ignored due to a lack of awareness. Some seek treatment from traditional healers, others have constraints such as inadequate access, costly health care, gender-related social barriers, and stigma around symptoms.
This may be attributed to their unawareness that what the lump represents, the stigma of being rejected by the community and partner, potential fear of loss of the breast, and the major obstacle being the prevailing taboo of not discussing breast cancer topic openly, and disbelief of the existence of any effective therapy for the disease.
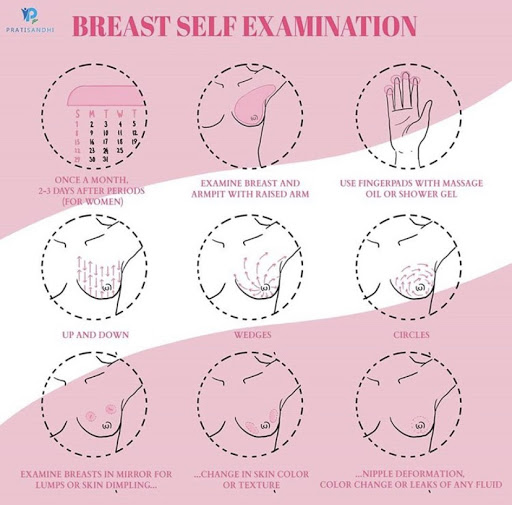
According to the American Cancer Society, when breast cancer is detected early and is in the localized stage, the 5-year relative survival rate is 99%. Early detection includes doing monthly breast self-exams and scheduling regular clinical breast exams and mammograms. We recommend talking to your doctor/medical experts to find out more about the same because early diagnosis can give us an increased number of treatment options, increased survival, and improved quality of life.
Self Examination?
Although there is quite a lot of debate about self-examination tests being futile, many do believe that it’s a useful screening tool, convenient and no-cost.
Dr. Nancy Baxter, the lead author on a study conducted to find out whether self-examinations do more harm than good, said that even though the technique had been promoted for 30 years, only about a third of women practiced it monthly, while even fewer did it properly. Harm could be caused by anxiety and unnecessary biopsies.
While no single test can detect all breast cancers early, it is believed that performing breast self-exam in combination with other screening methods can increase the odds of early detection. Additionally, self-examination is a vital step towards becoming more aware of the telltale signs of breast cancer, making it an easier option for increasing awareness amongst those who do not have the resources to choose any other.
We, at Pratisandhi, shared a guide to self-examination too!
Who is at risk?
For a country like India with a huge population, diverse cultures, geographical variations, diets, and habits, sources of information on cancer risk factors are considerably limited. The reasons for varying incidence of breast cancer among women are not fully understood, which are likely to be explained by reproductive and lifestyle factors such as literacy, diet, age at menarche and menopause, age at first delivery, abortion, and family history of breast cancer.
BreastCancer.org shares some risk factors that we’ve summarised for you!
Gender. Being a woman is the most significant risk factor for developing breast cancer. Although men can get breast cancer, too, women’s breast cells are constantly changing and growing, mainly due to the activity of the female hormones.
Age. Simply growing older is the second biggest risk factor for breast cancer. In a study conducted to establish data regarding breast cancer in India, it was found that breast cancer seems to be more common in the younger age group in India and 52% of all women suffering from breast cancer in Mumbai are between 40 and 49 years of age.
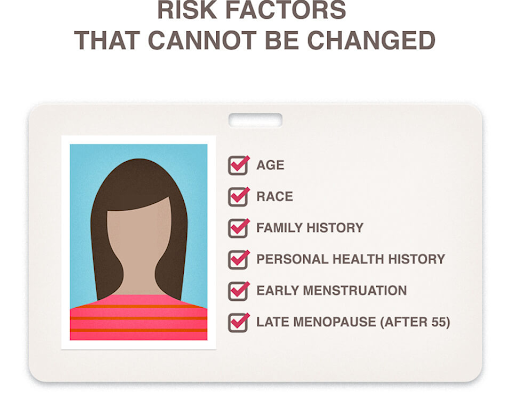
Family history of breast cancer. Having a family history of breast cancer, particularly women with a mother, sister, or daughter who has or had breast cancer, may double the risk.
Exposure to estrogen. Women who start menstruation at an early age (before age 12) and/or menopause at an older age (after age 55) have a slightly higher risk of breast cancer. The increase in risk may be due to longer lifetime exposure to the hormones estrogen and progesterone.
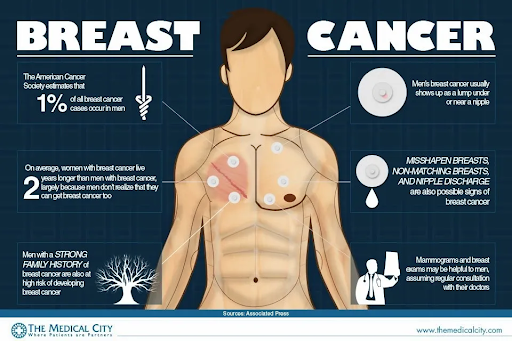
Breast cancer in men?
All people, whether male or female, are born with some breast cells and tissue. Even so, male breast cancer is very rare. Less than one percent of all breast cancer cases develop in men, and only one in a thousand men will ever be diagnosed with breast cancer.
There is a clear imbalance in the way we look at men and breast cancer. The reason is that though they do not develop milk-producing breasts, they do have small amounts of breast tissue that can become cancerous. The high mortality rate in men with breast cancer is attributed to poor awareness about the condition in men. This leads to men taking it too lightly and getting diagnosed for the condition often in its later stages. Various conditions can lead to an increased risk of breast cancer in men, such as conditions that increase estrogen levels in their bodies, such as liver disorders or the age, where men after the age of 60 become more susceptible to the disease.
Trans Women and Breast cancer
Trans women using hormone treatment and synthetic breast implants show an increased risk of breast cancer.
Data on the risk of breast cancer in transgender people is limited. In a study conducted in the Netherlands in 2019, it was found that transwomen have a 46-fold higher chance of getting the disease compared to a cis-gender man.
Screening in India, even for cis-gender women mostly happens at a later stage, which as we’ve highlighted in our article is one of the main causes of death due to breast cancer, for trans women in India there’s almost no data and resources made available.
In an interview with RE-Set, Dr. Bharat Vaswani, a Hyderabad-based oncologist, said that not enough studies are conducted on the risk of breast cancer among trans women. “I’ve treated some men with breast cancer but never a trans woman suffering from breast cancer,” Vaswani explained. “No one has evaluated this properly. We don’t have any data on this, and due to the low number of people going through HRT, it’s difficult to conduct a study. Theoretically, the risk in trans women should increase due to an increase in estrogen levels from HRT.”
In October, Bangalore’s HCG Cancer Care, a leading Indian cancer treatment group with 27 locations, invited hijras to be part of a unique public service campaign about breast cancer prevention called “Love Your Breasts. Or Lose Your Breasts.” The campaign utilizes posters, billboards, and a short film to raise awareness.
Various measures can be taken to increase awareness, government agencies, non-government organizations, and the media can play a major role in increasing awareness about breast cancer among the general public. Awareness campaigns in regional languages will have better penetration. Women in late thirties should be the target to screen in India as breast cancer is occurring in the younger age group over here. But, India is a country with limited resources and there are many cultural, social, and health infrastructure differences, therefore, we should form our management guidelines which are feasible and practical.
As of now, we hope our readers learn something from this article and do their part to increase awareness, for all we know, we could be saving lives with just a simple discussion.
Featured Image Credits: CompleteWomenCare
Author

